Left bundle branch block (LBBB) is important to identify because:
- it is associated with increased mortality
- it is usually caused by heart disease (but not always)
- it causes diagnostic interference with myocardial ischemia, myocardial infarction, and LVH due to the fact that all these diagnoses result in changes to the QRS, ST segment and T wave
Before listing the diagnostic criteria for LBBB, let's see if we can picture what is happening:
We will start with a CT scan of the chest:
And let's add V1 and V6 leads:
We are looking at the heart in this orientation because the diagnosis of bundle branch blocks are mostly made in the precordial leads, primarily Leads V1 and V6. Remember that these leads measure electrical activity in the axial plane, so looking at the heart in the axial plane might help you understand better. Remember that this is the axial plane:
Important - note the orientation of the RV and LV in the chest:
With LBBB, the RV will be depolarized first:
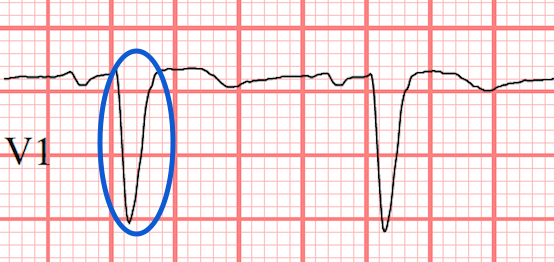
This will send an electric signal toward V1 and we often (but not always) see a small upgoing deflection in V1 (which is a small R wave):
After this, the LV SLOWLY depolarizes:
Because the conduction will be slow, the QRS waveform will be wide. This forms the basis of one of the diagnostic criteria: QRS > 120 ms.
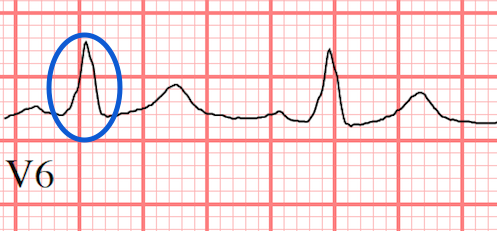
Electrical activiation is moving toward V6 (and away from V1). This produces an R wave in V6. Since V5 and lead I and aVL are very similar to V6, we would expect to see the similar pattern in these leads too and they are often also included in the diagnostic criteria for LBBB. Moving away from V1 produces an S wave in V1:
As the R wave is produced in V6, it will be produced slowly. The intrinsicoid deflection is the time required from start of QRS to peak of R wave. This is also called the R peak time. With LBBB, the intrinsicoid deflection is abnormally long or delayed. The diagnostic criteria is intrinsicoid deflection > 60 ms (remember 1 little box = 40 ms, so it 1.5 little boxes). Here is an example (the blue lines): 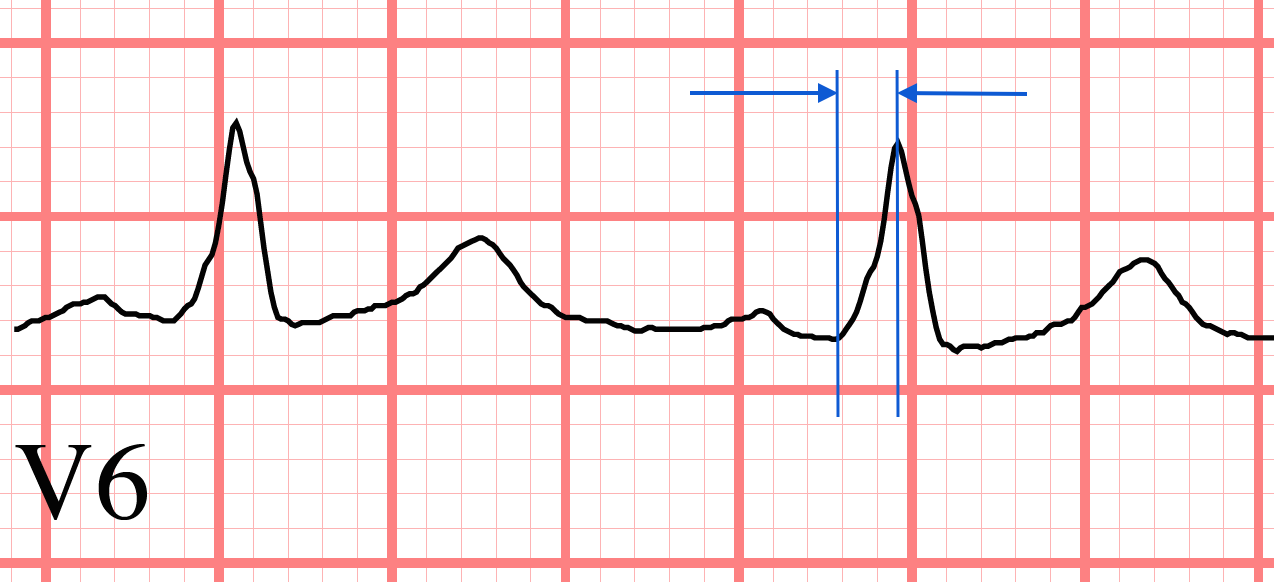
ST Segment and T wave changes:
Remember that normal repolarization is from epicardium (outer layer) to endocardium (inner layer); the exact opposite of depolarization. This normal pattern is lost in LBBB. The wave of repolarization follows the same direction and pathway as depolarization because the conducting fibers are not being used.
Remember that repolarization is the electrical opposite of depolarization. Therefore, the T wave in LBBB will be in the opposite direction as the QRS, since they are both travelling in the same direction. This is called discordance.
Similarly, if there are any changes in the height of the ST segment, they typically are also discordant. In the following image, we have shown blue arrows indicating the direction of the QRS and red arrows showing the discordant T waves:
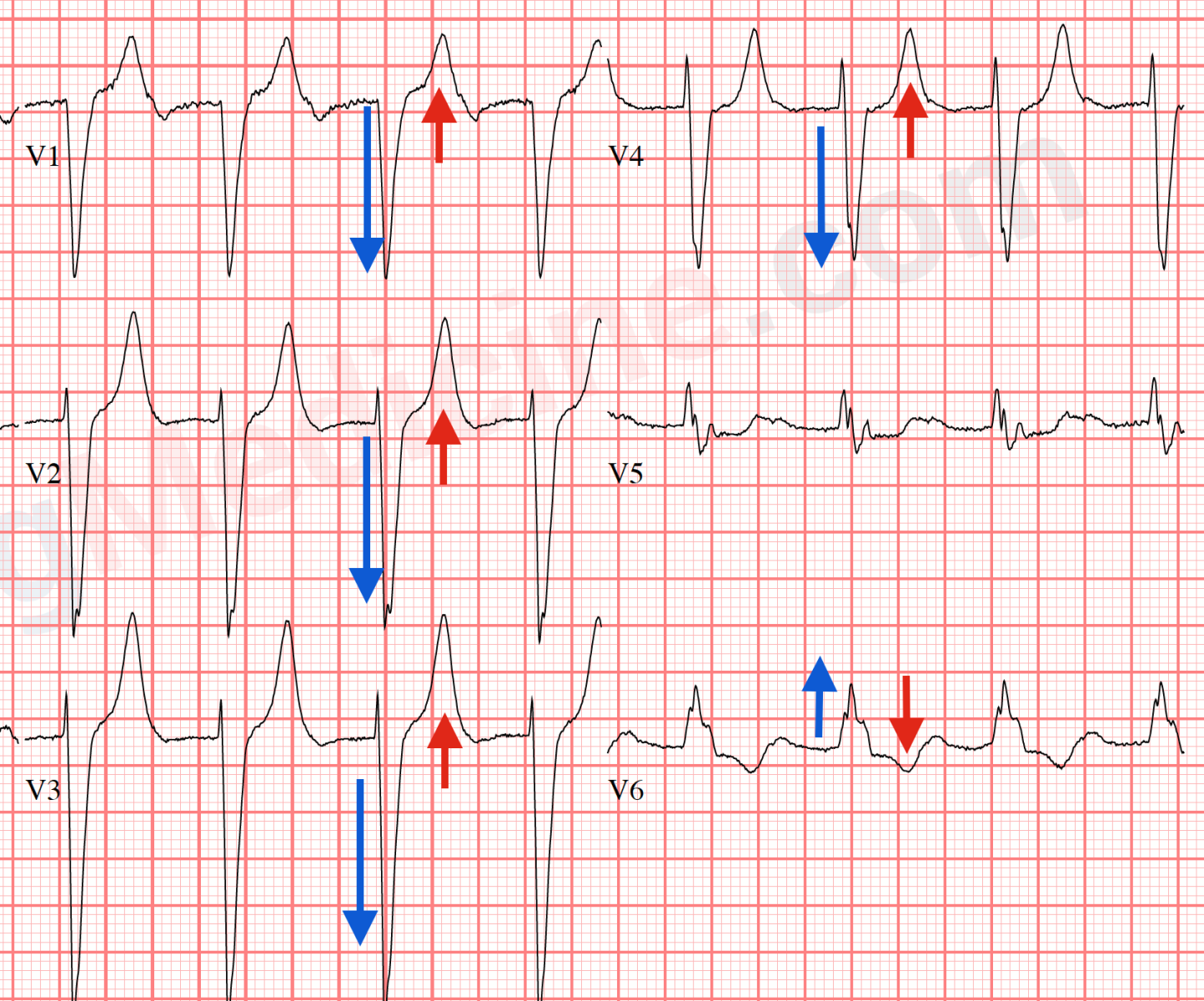
This discordance is the basis upon which LBBB alters the ST segment and T waves. This causes diagnostic interference with myocardial infarction and ischemia. In the above example, V5 shows a QRS that is nearly isoelectric so the discordance is difficult to see in that lead.
Summary of Diagnostic criteria for LBBB:
- QRS > 120 ms
- broad (wide) R wave (upgoing wave) in V6 (also in leads I, aVL and V5)
- small R wave, big S wave (also called rS) in V1
- QRS and T waves are in opposite directions (discordance) in most/all of the precordial leads
- (optional but not required) intrinsicoid deflection > 60 ms in V6
- (notice there are no Q waves in precordial leads)
Exceptions to the rules:
- sometimes the QRS and T waves can both be upgoing ("positive" concordance).
- sometimes there is an R + S wave in V6 instead of just an R wave. Late LV depolarization AWAY from V6 causes the S wave (see image).
- in children, the QRS duration criteria is > 100 ms. in ages 4-16 and > 90 ms. in ages < 4 yrs
Can you be a rock star and identify all 5 diagnostic criteria in the following ECG? Can you remember the logic and explanations for each of these diagnostic criteria?
Reference:
Surawicz B, et al. American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology, American College of Cardiology Foundation, Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009;119:e235-e240