Lesson 4: Leadership/Followership 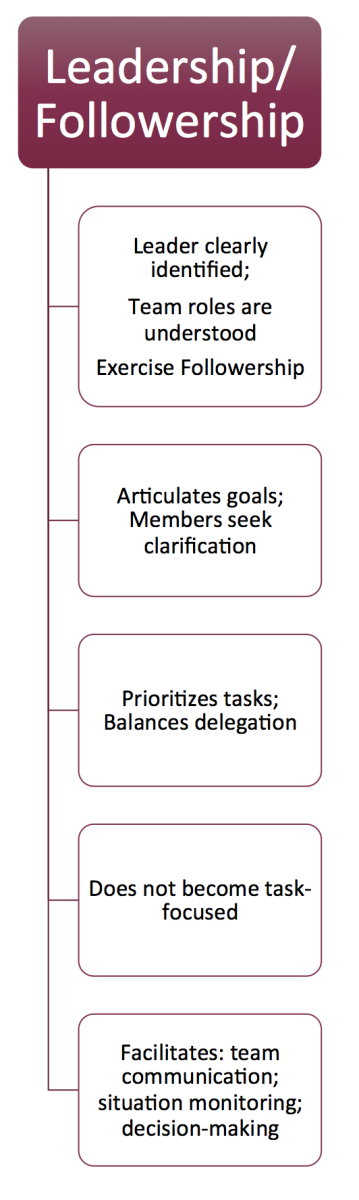 At the end of this module, you will:
At the end of this module, you will:- Understand the elements of Leadership/Membership
- Consider specific teamwork strategies to improve leadership/membership
- Consider examples of how you might apply effective leadership and membership skills to clinical practice
The Leader is clearly identified; team roles are understood Using direct communication is important to clearly identify roles including the leader and other team members. Establishing clear leadership is especially important during times of handover, or when two or more potential leaders are attending to the same patient.
For Example:- Who is the leader when a trauma surgeon arrives into the trauma bay while the emergency physician is ordering the xrays?
- Who is the leader in a community care clinic where a patient collapses in the waiting room–the Nurse Practitioner who is there every day or family physician attending that morning?
Time for Reflection: What opportunities exist on your team to clearly identify roles in advance?
Key Point:It is the responsibility of every team to clarify their role as well as that of the others. A team member must exercise good “membership (followership)”. If you are unclear on leadership, then ask…there’s a good chance that you are not the only one needing the clarity on roles. Exercise Followership:Followership is defined as the capacity of a team member to actively follow a leader. Followership is also important to the performance of a team and involves the ability to take direction, deliver what is expected of you within your role, and make good judgments. (10)
This means that a good follower will speak up if they believe the direction they are being given is not correct or is a risk to patient, staff or team safety. They also need to speak up if they are not comfortable with the role they have been delegated, are unsure of how to preform a task, need help, or are feeling overwhelmed.
The Leader articulates goals and members seek clarification: We have reviewed the power of “huddling” or summarizing for the team to keep everyone “on the same page”.
The goal for the team needs to be articulated and sometimes needs revision as the situation evolves. Team members should seek clarity if the goals are not clear.
For Example:The leader may state, “My goal here is to stabilize the blood pressure with fluids before we move him to the CT scan. I think he is dry so I’m going to try 3 liters of saline before we consider vasopressors. I agree that the scan is very important and we can do that just as soon as his systolic blood pressure is above 90”.
This type of goal setting allows the team to anticipate the next steps. For example, someone could then ask, “Have we called CT scan to see if they can accommodate him?”
Leader prioritizes and balances tasks: Mistakes can happen when team members become overwhelmed, fatigued or practice outside of their skill set.
Key Point:Speaking up can be difficult! If you feel you can’t perform a task as requested for whatever reason (overburdened, unqualified, fatigued), you must speak up for the best patient outcome. Leaders should also reinforce this message with the team.For Example:A leader asks for three intravenous drugs in rapid succession (each requires a calculation and being drawn up/diluted and administered). The nurse should speak up to ensure that the leader knows that these drugs will take some time and that administration can be expedited if another nurse can be assigned to help with this task.
In such a situation, the leader will then have to prioritize tasks for both the available RNs, or see if more resources are available.
Leader must not become task focused Focusing your attention on a specific task (e.g. preparing for intubation, analyzing a blood gas or ECG, etc.) is essential for success. However, if you need to focus on a task, you cannot reliably see the “whole team” or maintain the “big picture”. If the leader loses this global awareness, there can be a failure to appreciate the passing of time, the overall team performance or changes in patient status. (11)
It is critical that one person (ideally the leader) remains “hands free” to avoid becoming overly fixated on one task. Some experienced leaders specifically position themselves away from the action (e.g. at the foot of the bed) with hands behind their back to avoid the temptation of being too “hands-on”. If this isn’t possible and the leader needs to focus on a single task ( for example when the leader is the only one with skills to intubate) then another team member needs to take on the leadership role of maintaining the “big picture”.
Key Point:Leadership can transition at any time during a team experience. Transition must be explicit for the rest of the team! Leader facilitates Team Communication, Situation Monitoring and Collaborative Decision Making: Once two or more people come together to form a team, there needs to be a designated “leader” whose key role is to keep the team progressing towards the end goal.
“Team Members” are equally important, as they need to recognize the responsibilities of the leader and support this role. Being the leader is difficult and is only successful with good membership/followership.
Leaders do not necessarily have all answers but they FACILITATE good team work to reach end goals.
Key Point:Everyone on the team is equally responsible for the patient’s safety and well being!Time for Reflection:How does a good leader create psychological safety on a team so that members feel comfortable speaking up for patient safety, contributing to the mental model and fulfilling their critical “membership” roles?